A Report Series on Lessons Learned From PEPFAR’s Success
Introduction
The President’s Emergency Plan for AIDS Relief (PEPFAR) forged a new path for pandemic response from its inception. Because of the leadership of President George W. Bush and the U.S. Congress, PEPFAR has employed a whole-of-government approach that leverages the strengths of individual departments and agencies to accelerate outcomes. PEPFAR has used real-time data to constantly improve programmatic results. It has focused on increasing impact and achieving the third United Nations sustainable development goal of ensuring healthy lives and promoting well-being for all at all ages.
Over the past two decades, PEPFAR has created a series of public-private partnerships (PPPs) to improve its results and sustainability – collaborative working relationships with nongovernmental partners guided by mutually determined goals, structure, governance, roles, and responsibilities. These PPPs have changed as PEPFAR has identified new programmatic gaps and barriers, and their continual evolution has added to the program’s success.
Partnerships of this nature are particularly valuable to a large-scale, highly collaborative initiative such as PEPFAR. When designed and implemented well, PPPs can help expand the reach and impact of interventions; better allocate risk between public and private entities; and bring greater efficiency and sustainability to the provision of HIV/AIDS prevention, care, and treatment. The private sector has invested hundreds of millions in PEPFAR’s programs since its inception. But the money is only a small part of the partnerships. The value lies in the private sector’s unique insights and approaches, which improve outcomes and impacts. PEPFAR partnerships have done the following:
- Advanced a shared objective;
- Enhanced impact through resource sharing;
- Improved the programmatic reputation/visibility of both PEPFAR and its partners; and
- Achieved mutual programmatic goals.
This paper explores the critical role of PPPs in the broader PEPFAR ecosystem. It highlights notable partnerships – many of which are still active today – that have made significant contributions to the program’s impact and provided examples of success that other U.S. foreign assistance initiatives should emulate.
This paper is part of a series that examines the lessons learned from PEPFAR and their implications for U.S. engagement in global health and development. The first paper covered the important role of the collection and continuous analysis of data to manage programs. The second assessed PEPFAR’s critical collaboration with multilateral organizations to achieve the goal to end AIDS by 2030. The third provided an overview of PEPFAR’s use of innovative GIS technology to advance program equity. The fourth offered an in-depth look at how PEPFAR has deployed data to identify communities and demographics that have been left out of care and used innovative approaches to further access to care for all. The fifth showcased the centrality of communities to PEPFAR’s success and long-term sustainability.
Traits of Successful Partnerships
PEPFAR did not create any of its PPPs in isolation, but rather initiated each of them to address persistent gaps in prevention, care, and treatment services for specific risk, gender, or age groups. All the partnerships evolved based on programmatic data.
PPPs are important to PEPFAR for four reasons:
- They bring in additional resources to meet PEPFAR’s goals. PPPs bring in cash or in-kind resources that effectively expand the program’s budget at no cost to the American taxpayer – unlike any other part of PEPFAR.
- They provide valuable expertise not available within the U.S. Government.
- They strengthen systems and local capacity – for example, through training of clinicians and health workers around patient care and treatment protocols, building laboratory services and infrastructure, and increasing supply chain know-how. These activities enable the local private sector and government entities to build more sustainable business operations and to better leverage business opportunities.
- At a time when PEPFAR is focused on sustainability, PPPs often provide a strategy for transitioning the relationship. While we cannot say for certain how long PEPFAR programming will persist, companies are looking toward developing countries for long-term growth, and their commitment and presence will endure.
- In many countries, including the United States, the private sector can play a key role in advocacy for the fight against HIV, for health in general, and against discrimination and other barriers to lifesaving services. Engaging directly with the private sector has been an important component of keeping HIV on global, national, and local agendas.
By using the skills, resources, and access that the private sector provides, PEPFAR can help to make its programming more effective and reach greater numbers of people.
PEPFAR’s successful PPPs share the following characteristics:
- Clarity that the clients’ needs are the primary focus of the partnership;
- A shared commitment to well-defined, measurable outcomes with clear impact;
- A willingness to listen and take a solution-focused approach;
- Flexibility and adaptability to ensure the program meets the needs of all stakeholders;
- A commitment to collect data in real time and use it to improve programmatic implementation on a continuous basis.
At their best, PPPs are effective in extending the impact of a program, leveraging the talents and expertise of diverse partners to tackle a common problem. Additionally, PEPFAR has created lasting connections through PPPs that strengthen overall health care delivery capacity, creating an ecosystem of care with benefits that continue to extend beyond PEPFAR’s scope (e.g., helping with containment of the Ebola epidemic in West Africa).
Initial Role of Public-Private Partnerships
The legislation that codified PEPFAR into statute, the United States Leadership Against HIV/AIDS, Tuberculosis, and Malaria Act of 2003 (Public Law 108-25), provided a broad mandate for the program to create public-private partnerships, as shown below.
- FINDINGS.—Congress makes the following findings:
- Innovative partnerships between governments and organizations in the private sector (including foundations, universities, corporations, faith-based and community-based organizations, and other nongovernmental organizations) have proliferated in recent years, particularly in the area of health.
- Public-private sector partnerships multiply local and international capacities to strengthen the delivery of health services in developing countries and to accelerate research for vaccines and other pharmaceutical products that are essential to combat infectious diseases decimating the populations of these countries.
- These partnerships maximize the unique capabilities of each sector while combining financial and other resources, scientific knowledge, and expertise toward common goals which neither the public nor the private sector can achieve alone.
- Sustaining existing public-private partnerships and building new ones are critical to the success of the international community’s efforts to combat HIV/AIDS and other infectious diseases around the globe.
- SENSE OF CONGRESS.—It is the sense of Congress that —
- the sustainment and promotion of public-private partnerships should be a priority element of the strategy pursued by the United States to combat the HIV/AIDS pandemic and other global health crises; and
- the United States should systematically track the evolution of these partnerships and work with others in the public and private sector to profile and build upon those models that are most effective.
Members of Congress realized that working with the private sector would provide PEPFAR with significant access and distribution points for the delivery of services through innovative and efficient ways to reach the populations most affected by the epidemic.
At the same time, the global HIV/AIDS epidemic was becoming an acute concern for multinational corporations and local businesses in affected countries as rising levels of infection and death were jeopardizing both their workforces and consumer bases. As a result, the private sector responded enthusiastically to the call to work with PEPFAR.
PEPFAR started relationships with the private sector through the U.S. Chamber of Commerce and country-specific opportunities identified by U.S. embassies. Larger-scale efforts began in earnest with the establishment of the Office of Private Sector Engagement within the Office of the U.S. Global AIDS Coordinator at the U.S. Department of State (SGAC), which became responsible for spearheading and maintaining public-private partnerships at international, national, and enterprise levels.
PEPFAR has developed hundreds of partnerships over the last 20 years. Many were successful and continue today; others proved more challenging. All of them, however, provided valuable lessons that have shaped future PPPs. The partnerships highlighted below are among the most successful in achieving impact and sustainability and are models for future efforts in U.S foreign assistance.
Labs for Life
A strong laboratory system is critical to supporting prevention, treatment, and care interventions and fundamental to the success of efforts to combat the spread of HIV/AIDS. Clinicians rely on laboratory data to make accurate diagnoses, formulate treatment plans, and monitor the effects of treatment. Laboratory results must be accurate, readily available, and timely.
To bridge the enormous gaps in existing laboratory systems, PEPFAR – through the Centers for Disease Control and Prevention – launched a first-of-its-kind partnership with global medical technology company Becton, Dickinson and Company (BD) to improve overall laboratory systems and services in African countries severely affected by HIV/AIDS and tuberculosis.
Upon its initial launch in October 2007, the Labs for Life partnership provided $18 million for eight African countries: Côte d’Ivoire, Ethiopia, Kenya, Malawi, Mozambique, South Africa, Tanzania, and Uganda. The partnership’s implementation strategy focused on three key components developed in collaboration with ministries of health, national reference laboratories (NRLs), and implementing partners: country-specific laboratory strengthening programs based on national laboratory strategic plans; fellowship programs for BD’s in-house experts to work closely with implementing partners, ministries, and NRLs; and short-term technical assistance by both BD and PEPFAR partners to provide laboratory training and develop a framework to improve all levels of laboratory service.
A third-party assessment of this PPP after its initial five years showed that countries where the partnership worked to build capacity had not only improved the quality of services available to local populations, but also had become regional centers of excellence in Africa.
In July 2012, the partners built on their successful collaborative efforts to launch Labs for Life – a five-year agreement that included Uganda, Kenya, Ethiopia, and Mozambique, and, later, India. This second phase focused on quality improvement, training on pathology and equipment maintenance, strengthening local capacity and promoting country ownership and sustainability, using systems originally designed for HIV to address noncommunicable diseases, and creating capabilities in health facilities to adopt point-of-care technologies.
Now in its third phase, PEPFAR’s Labs for Life partnership with BD is providing continuous quality improvement, strengthening human resources in laboratories, helping to prevent tuberculosis, and improving systems for transporting and referring specimens.
Building Tanzania’s Laboratory Capacity
PEPFAR’s investments in laboratory capacity also included an infrastructure-focused partnership with Abbott to enhance the availability and quality of diagnostics in Tanzania. Recognizing that inadequate laboratory services were the weakest link in the provision of quality HIV/AIDS care and that PPPs can facilitate the implementation of rapid changes, PEPFAR developed a partnership between Tanzania’s Ministry of Health and Social Welfare (MOHSW), CDC-Tanzania, Abbott Fund Tanzania, the Association of Public Health Laboratories (APHL), and not-for-profit health care design firm Design 4 Others (D4O).
The MOHSW and CDC coordinated partners’ contributions and served as a liaison between partners, leadership, and laboratory medicine experts. In addition to funding, Abbott provided experience and resources in laboratory renovation and project management. APHL and D40 brought extensive expertise in laboratory design to the partnership.
The partners collaborated to build and modernize 23 regional-level laboratories throughout Tanzania and to build an outpatient center at the national referral hospital in Dar es Salaam that serves 1,000 patients per day. Within the first five years, the partnership generated a 10-fold increase (from 110,000 to 1.158 million) in test volumes, which improved health care for people living with HIV and demonstrated proof of concept for a cost-effective nationwide laboratory improvement project.
Expanding Access to Rapid TB Testing
Tuberculosis is the leading cause of death among people living with HIV in Africa. Traditional testing methods severely limited clinicians’ ability to diagnose and treat TB in patients coinfected with HIV in an accurate, cost-effective, and timely manner. To address this gap, PEPFAR formed a partnership with the U.S. Agency for International Development (USAID), global health agency UNITAID, and the Bill & Melinda Gates Foundation to reduce the cost of a new, highly accurate, rapid diagnostic test for TB in 145 high-burden and developing countries.
Previously, the high unit cost of these testing supplies had proven a barrier to their introduction and widespread use in low- and middle-income countries. Funds provided by this PPP lowered the cost of testing supplies produced by medical device manufacturer Cepheid by more than 40%. At the time, research suggested that the incremental scale up of Cepheid’s GeneXpert diagnostic system could allow for the rapid diagnosis of 700,000 cases of TB and save governments and private providers more than $18 million in direct health costs.
This PPP was significant because it leveraged the role of PEPFAR as a major funder in derisking research and development to accelerate product availability in local markets at much lower costs.
Expanding Prevention Interventions for Youth, Shuga
An innovative partnership with the entertainment industry has been one of PEPFAR’s most successful education initiatives to date. To prevent infection and promote healthy behaviors among young adults, PEPFAR partnered with the MTV Staying Alive Foundation to produce a multimedia campaign that featured a groundbreaking Kenyan TV-radio series, Shuga, as a stand-alone spinoff of PEPFAR’s HIV-Free Generation partnership with Accenture, Coca-Cola, Kenya Girl Guides (known as Girl Scouts in the United States), the Global Business Coalition, Hasbro, Intel, Microsoft, MTV, Nike, and Warner Bros. The show, which included Academy Award-winning actress Lupita Nyong’o in its initial cast, has combined data-driven insights with compelling storylines to influence the behaviors of its target audience since premiering in 2009.
In addition to becoming an award-winning sensation, Shuga has made a substantial impact in the fight against HIV/AIDS, as documented in two World Bank studies. The first, conducted between 2014 and 2018, found that HIV testing doubled among 5,000 young people who watched the show in Nigeria. Additionally, cases of chlamydia in female viewers decreased by half, as did the number of respondents who reported having multiple concurrent sex partners.
A subsequent cost-benefit analysis in 2017 determined that one season of the show saved more than $300 million across five countries over 30 years compared with alternative ways of expanding community awareness.
Today, Shuga continues to air across dozens of countries. In 2022, the MTV Staying Alive Foundation announced the launch of three new MTV Shuga campaigns across Nigeria, South Africa, and India, which will use this successful platform to tackle other pressing health and social issues, including tuberculosis, COVID-19, and mental health. An American version of Shuga is also set to begin production in Baltimore, Maryland, the first time a PEPFAR-funded communications vehicle will come to the United States.
Addressing Gender Based Violence, Together for Girls
PEPFAR has long been committed to reducing vulnerability to HIV infection by both addressing the structural drivers of violence and HIV for women and girls and advancing their health and rights. Together for Girls (TfG) is a pioneering partnership between public and private organizations, U.N. agencies, and the U.S. Government that addresses violence against children.
Launched in 2009, the partnership brought together private sector organizations, including the Nduna Foundation, BD, the CDC Foundation, and Grupo ABC; five U.N. agencies, including UNICEF, UNAIDS, U.N. Population Fund (UNFPA), UN Women, and the World Health Organization (WHO); and the U.S. Government, through the CDC’s Division of Violence Prevention and PEPFAR.
TfG is dedicated to breaking the cycle of violence against children, with special attention given to sexual violence. The partnership was designed to coordinate and leverage resources from its founders and other donors, with activities focused on three pillars:
- Conducting national surveys to document the magnitude of violence against children;
- Supporting coordinated programmatic actions at the country level in response to the data; and
- Leading global advocacy efforts to raise awareness and promote evidence-based solutions.
With support from TfG partners, National Violence Against Children Surveys have been completed in countries including Swaziland, Tanzania, Kenya, Zimbabwe, Haiti, Malawi, and the Philippines. In 2012, PEPFAR announced a $5 million investment in the TfG partnership to support national responses to the data generated by the TfG surveys. As a result, ministries and advocacy organizations have developed programs and interventions to address the underlying social determinants of sexual violence against children and better support survivors.
Today, TfG continues as a stand-alone entity with its own board of directors and uses an innovative model of data, advocacy, and action to drive lasting change. Donors contribute at least $20 million worth of resources to the partnership’s work each year, and TfG has leveraged more than $100 million of direct and in-kind resources over the past 14 years to achieve its goals.
Supporting Global Initiatives: Eliminating Mother-to-Child Transmission
PPPs can take many forms, from governments engaging local private health associations to expand access to quality services to multinational corporations working alongside governments to advance technical training, capacity building, and access to new technologies. These matchups allow the public and private sectors to work together to combine and coordinate their unique human and financial resources.
At the 2011 U.N. High Level Meeting on HIV/AIDS, Chevron partnered with PEPFAR and UNAIDS to support the Global Plan Towards the Elimination of New HIV Infections Among Children by 2015 and Keeping Their Mothers Alive. Chevron committed $20 million to support the plan, and PEPFAR increased its investments in the prevention of mother-to-child transmission (PMTCT) of HIV by a total of $75 million over the following three years.
As part of this $20 million commitment, Chevron worked with the Business Leadership Council and Nigeria’s Federal Ministry of Health on an ambitious prevention of mother-to-child transmission (PMTCT) scale-up program and with the NGO Pact in Bayelsa State, Nigeria, on a program to eliminate the mother-to-child transmission of HIV.
Since 2008, Chevron has contributed over $60 million in Nigeria to support PMTCT, reduce new HIV infections, and improve the quality of life for the infected and those affected by the disease.
Improving Food Processing in Africa
PEPFAR announced a PPP with General Mills and USAID in September 2009 to improve the capacity of small and medium-sized food businesses across sub-Saharan Africa. The goal was to produce healthy, fortified food products at affordable prices for HIV/AIDS patients and their families.
High-quality nutrition is crucial to increasing the number of people living with HIV who start and stay on lifesaving antiretroviral treatment (ART). PEPFAR programs prescribe therapeutic and supplemental foods for severely malnourished patients to ensure the effectiveness of treatment. The problem is many countries rely on expensive food imports. This PPP has improved the ability to source foods locally, stimulated local economies, and promoted food security in areas heavily affected by HIV/AIDS by linking the technical and business expertise of General Mills and other food companies with up to 200 small and medium-sized mills and food processors in 15 sub-Saharan African countries.
This PPP continues today under the oversight of Partners in Food Solutions, an independent, nonprofit organization that links corporate volunteers from its consortium of leading food companies with promising entrepreneurs in 12 African countries.
Addressing the High Risk of Cervical Cancer Among HIV-Positive Women, Evolution of Pink Ribbon Red Ribbon to Go Further
During the Bush Administration, clinicians in Zambia informed SGAC that they were seeing young women and girls with HIV who had developed aggressive cervical cancer, including ones on ART. Young women without HIV did not have the disease. It became clear that cervical cancer, caused by the human papillomavirus (HPV), was a deadly consequence of the damage to women’s immune system caused by HIV. ART was saving women’s lives initially by arresting the progression of HIV into AIDS but could not stop HPV from causing cancer.
However, a relatively easy, affordable, and effective approach existed to screen for the lesions caused by HPV and treat them before they advanced into cancer. Because PEPFAR already was funding interventions to prevent and treat tuberculosis, another so-called “opportunistic infection” that takes advantage of HIV’s ability to weaken human immunity, the team at CDC in Zambia proposed using PEPFAR funds to attack cervical cancer. Given that precedent, the U.S. Global AIDS Coordinator authorized a pilot program in Zambia to screen women for early cervical precancer and use liquid nitrogen to freeze off any abnormalities found. The local partner, the Centre for Infectious Disease Research in Zambia (CIDRZ), had gained expertise in HPV and cervical cancer because of work done under research grants from the U.S. National Institutes of Health. By the conclusion of the pilot in 2010, CIDRZ had shown that women living with HIV are up to six times more likely to develop cervical cancer and can succumb to it despite having survived HIV. The pilot also proved that cervical cancer is curable if detected early enough, even in HIV-positive women in lower-income countries.
But the services and tools required to detect and treat cervical cancer were not available in most places where PEPFAR worked. In contrast, most high-income countries had virtually eliminated aggressive cervical cancer through childhood vaccination programs against HPV and regular screening for precancerous cervical lesions.
To address this inequity, the George W. Bush Institute, PEPFAR, Susan G. Komen and UNAIDS decided to build on the Zambian proof of concept by forming a PPP to address breast and cervical cancers – the top cancer killers of women in Africa.
President and Mrs. Bush announced the new partnership, called Pink Ribbon Red Ribbon, alongside Secretary of State Hillary Clinton at the 2011 Summit to Save Lives in Washington, D.C. The launch demonstrated the continuation of PEPFAR’s impact across successive administrations and one of its crucial lessons for success – bipartisanship.
The founding partners mobilized additional foundations and private sector companies to leverage resources to screen and treat precancerous cervical lesions and deliver vaccines against HPV. Over five years, Pink Ribbon Red Ribbon established programming in Botswana, Tanzania, and Zambia, where PEPFAR was the primary source of funds, and in Ethiopia, largely funded through a corporate grant. The Bush Institute hosted the partnership’s small full-time staff (called the “secretariat”). Pink Ribbon Red Ribbon did not open offices overseas.
Pink Ribbon Red Ribbon’s partners screened more than 500,000 women over five years across the four countries, over 400,000 of whom were screened for the first time in their lives. Almost 120,000 of these screenings were among women living with HIV. Over 147,000 girls under age 13 were vaccinated against HPV, which causes cervical cancer.
Despite these results, the partnership struggled to meet its expectations for impact. After six years of implementation, only 2% of eligible girls across the four Pink Ribbon Red Ribbon countries had been vaccinated against HPV, and only 8% of the women in the eligible age range for screening for precancerous cervical lesions had received it. Moreover, women living with HIV were not being prioritized in keeping with the original intention of the partnership.
Members continued to join the partnership, but the cost in time and effort to manage them in many cases outweighed the benefits of their contributions. While partners signed memoranda of understanding that detailed millions of dollars in investments (especially through deep discounts or in-kind contributions), many were not fulfilled. Most important, the women who were meant to benefit from their unmet commitments continued to go without services.
Furthermore, without dedicated staff on the ground to oversee the implementation of Pink Ribbon Red Ribbon’s activities in country, the partnership often experienced challenges in making meaningful progress. Without cervical cancer indicators baked into the PEPFAR structure for data reporting, and with implementers often unsure who was beholden to oversee their progress, the Pink Ribbon Red Ribbon secretariat often experienced delays in receiving the data necessary to monitor the programs.
Despite the challenges Pink Ribbon Red Ribbon faced, the partnership did leverage millions of dollars in resources and in-kind contributions to support programs to fight cervical cancer. It succeeded in propelling awareness on the extraordinarily high burden of cervical and breast cancers that women in sub-Saharan Africa face. When it began in 2011, this problem was on almost no one’s radar. It pushed the WHO to develop new tools and policies to aid national governments to set up screening and treatment programs and worked with ministries of health to develop and evaluate cancer control plans. In 2018, Dr. Tedros Adhanom Ghebreyesus, Director-General of the WHO, made a global call to action to eliminate cervical cancer.
Recognizing the challenges and wanting to ensure maximum results, the Pink Ribbon Red Ribbon secretariat, SGAC, and the Bush Institute conducted a review of the results the partnership had achieved in its first six years and the needs that remained unmet. Together, they charted a course for the future of the partnership that would put it on a path to sustainability and impact.
Using estimates from Eswatini, a country with a significant burden of both HIV and cervical cancer, the Bush Institute and PEPFAR found that expanding HPV vaccination programs to HIV-positive women between the ages of 15 and 49 and offering screening for precancerous cervical lesions at the same time could reduce the incidence of cervical cancer by 95% within a generation in this population, as shown in Figure 1.
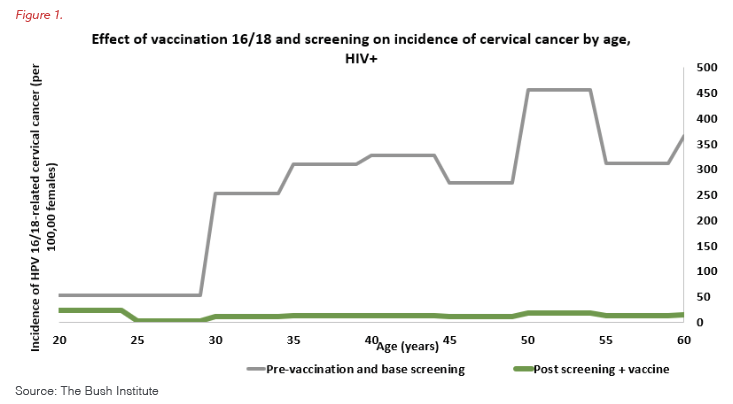
Using these estimates, the U.S. Global AIDS Coordinator advocated with Congress to appropriate dedicated funds through PEPFAR to accelerate screening and treatment for precancerous cervical lesions among women living with HIV in eight countries.
In 2018, President George W. Bush announced this new, more effective partnership, known as Go Further, founded by the Bush Institute, PEPFAR, and UNAIDS. Country teams got to work to scale up the programs at the beginning of the following fiscal year, which started in October 2018.
Within 12 months, the justification for the shift in the partnership’s structure became evident: Go Further screened more women in its first year than Pink Ribbon Red Ribbon had in six. At the same time, the partnership reached a greater percentage of women who had never been screened before.
As part of the Go Further partnership, PEPFAR now provides funding for the screening and treatment of precancerous cervical lesions in 12 countries in East and Southern Africa that have the highest burden of HIV among women of reproductive age. This investment has supported over 5.7 million screenings among women living with HIV, through the latest reporting period, which ended on Sept. 30, 2022. Moreover, the linkage-to-treatment rate has improved continually across all countries.
Women living with HIV are able to access screening and treatment for precancerous cervical lesions more easily through the PEPFAR infrastructure, as these services are often co-located in ART clinics. PEPFAR is able to track how many women on ART have received screening; what the results of the screening were; and if the women have been treated for precancerous lesions or cancer, if needed. PEPFAR recommends that women living with HIV be screened for cervical cancer every other year, a clear annual target for governments and their partners to screen half of all women on ART who are between the ages of 25 and 49.
PEPFAR has invested over $200 million in funding for activities related to cervical cancer. At the launch of PRRR, PEPFAR committed $30 million for five years, $20 million of previously planned resources combined with a new $10 million to match partners’ contributions. In 2015, PEPFAR announced an additional $7 million in funding for cervical cancer. Building off early success and an intention to focus efforts on women living with HIV, SGAC has significantly increased the available funding for cervical cancer, having contributed over $168 million in the last five years.
PEPFAR is responsible for the implementation, monitoring, and oversight of the screening and treatment of precancerous cervical lesions under Go Further. The Bush Institute leverages its convening power and leadership to help ensure commitment to the prevention and elimination of cervical cancer on the global level, manages the communications activities for the partnership, and works closely with PEPFAR and UNAIDS to recruit new members and promote new approaches to respond to gaps along the continuum of care. UNAIDS collects and shares data on indicators that track the implementation of cervical cancer policy and service integration; assists with formulating strategic and policy recommendations for national governments and partners; and engages civil society and communities in awareness raising, advocacy, and accountability. Merck provides an already-proven-effective HPV vaccine to a study to determine its safety and correct dosage in women living with HIV. Merck’s engagement with the partnership is helping Go Further make greater progress to prevent cervical cancer entirely. Roche assists ministries of health through a collaborative, multistakeholder approach that enhances access to high-quality tools, including digital and in-person navigation, to help patients improve the results of their journey through screening, diagnosis, and treatment.
Go Further is an example of how PEPFAR is tackling challenges that disproportionately affect women living with HIV, but PEPFAR cannot do everything. Gaps exist along the continuum of care that other partners must fill. Go Further recognizes a need to continue to make progress in eliminating cervical cancer through expanding the availability of the HPV vaccine, raising awareness among women living with HIV so they attend their recommended biennial screenings, and linking women who need treatment for precancerous cervical lesions with care. Better diagnostics and treatment for advanced cancers are a severely under-resourced area, which means that the chances of survival are slim for women who present with suspected cancer.
Evolution of Partnerships to Address Gaps in the HIV Treatment of Children From Scaling Up Pediatric HIV/AIDS Treatment to Accelerating Children’s Treatment (ACT)
In the absence of ART, 50% of children living with HIV die before their second birthday, and 80% die before their fifth birthday. Early initiation of treatment is known to lower mortality among children significantly. Throughout its first decade, PEPFAR made significant advances in access to ART for adults, but the treatment of children – especially those under age 14 – lagged significantly for several reasons. First, children are not just small adults, and many in-country clinical and medical officers were nervous about treating the youngest HIV-positive children. Second, many of the pediatric medications available were very difficult for children to take – especially the very young. Third, significant stigma and discrimination about HIV remained in communities, which created many barriers and difficulties for parents in obtaining the proper treatment for their children.
SGAC knew it had to galvanize the world to tackle this problem. On March 13, 2006, then-U.S. first lady Mrs. Laura Bush announced an unprecedented PPP, the Scaling Up Pediatric HIV/AIDS Treatment initiative, to promote scientific and technical discussions to find solutions for pediatric HIV treatment, formulations, and access. This partnership encouraged agencies across the U.S. Government to bring together a wide range of expertise from innovator and generic pharmaceutical companies; civil society organizations, such as the Elizabeth Glaser Pediatric AIDS Foundation and the Clinton Health Access Initiative; and the WHO, UNAIDS, and UNICEF. The PPP also worked to maximize the utility of currently available pediatric formulations and to accelerate children’s access to treatment. This approach complemented PEPFAR’s efforts to expand treatment for adults and children, such as support for health care capacity building and the expedited regulatory review of drugs through the U.S. Food and Drug Administration, which made eight new pediatric formulations available for PEPFAR-financed programs and the Global Fund to Fight AIDS, Tuberculosis, and Malaria.
Propelled by advancements in the availability of pediatric treatment achieved under the Scaling Up Pediatric HIV/AIDS Treatment initiative, PEPFAR ramped up the original PPP in 2014 to create Accelerating Children’s Treatment (ACT) in partnership with UNAIDS and the Children’s Investment Fund Foundation (CIFF). CIFF has contributed $50 million in addition to PEPFAR’s $150 million investment and collects the data on progress.
ACT’s mission is to create awareness and mobilize resources in a super-fast-track approach to the scale-up of HIV prevention, treatment, care, and support for children, adolescents, and young women. The partnership unites governments, foundations, and private sector partners to work through more than 100 implementing partners in nine African countries with the greatest need: Cameroon, the Democratic Republic of Congo (DRC), Kenya, Lesotho, Malawi, Mozambique, Tanzania, Zambia, and Zimbabwe.
Between 2014 and 2016, the number of children under 15 who received treatment under ACT through support from PEPFAR and CIFF increased by 44% across the nine countries. As of September 2016, the end of its two-year acceleration program, ACT was supporting 561,610 HIV-positive children and youth (19 years old or under) with access to high-quality treatment. But the partnership’s results are even more impressive than that: ACT doubled the number of children under 14 on treatment across all PEPFAR countries, as it not only raised awareness of the need but created a renewed commitment among governments, U.N. agencies, implementing partners, and the private sector to act together with urgency. As a result, ACT ensured that an additional 300,000 children have received lifesaving treatment who otherwise might not have survived.
Like the rest of PEPFAR’s PPPs, ACT achieved greater efficiencies, outcomes, and impact because it combined focus; a clear, data-driven mandate of need; and innovation and technical expertise. PEPFAR and CIFF shared a commitment to transparency, accountability, innovation, and scale, and they worked closely to plan and review programmatic results jointly. As a 2017 report published by PEPFAR and CIFF indicated, “ACT was a concerted, strategic, and ambitious response to the treatment gap among children with HIV.” ACT showed the power of PPPs and how increased focus and attention can lead to tremendous impact.
Addressing the Unique Risk of Girls, Adolescents and Young Women to HIV Acquisition – DREAMS (Determined, Resilient, Empowered, AIDS-Free, Mentored, and Safe)
Over the next few years, PEPFAR launched partnerships to address gaps in access among other populations at high risk of contracting HIV, notably young women and girls.
PEPFAR has developed a clear evidence base that shows adolescent girls and young women (AGYW) in sub-Saharan Africa remain disproportionately affected by HIV/AIDS: They represent 24% of all new HIV infections while making up only 10% of the population. HIV prevalence rates among females ages 15 to 24 are consistently higher than among their male peers, as AGYW are up to 14 times more likely to acquire HIV than males of the same age.
The reason for these disparities is that AGYW often face complex challenges and unique risks that place them at greater risk for HIV. For example, females in Uganda and Zambia are more likely to experience forced or coerced sexual initiation than males, and that is associated with negative health outcomes and HIV-risk behaviors. AGYW in Kenya and Zambia report high levels of sexual violence perpetrated by both intimate and nonintimate partners, which is associated with sexually transmitted infection (STI) and higher anxiety and depression. Additionally, AGYW in sub-Saharan Africa often experience early pregnancy and decreased access to secondary school and higher education. But data from Botswana suggest that HIV prevalence for women in their 20s drops significantly for each year of secondary schooling completed. So education is a part solution to prevent HIV among young women.
PEPFAR launched the DREAMS (Determined, Resilient, Empowered, AIDS-Free, Mentored, and Safe) Partnership with the Bill & Melinda Gates Foundation, Girl Effect, Johnson & Johnson, Gilead Sciences, and ViiV Healthcare on World AIDS Day 2014. The PPP’s goal is to reduce new HIV infections in AGYW between the ages of 15 and 24 who live in the highest HIV-burdened communities.
Many of the studies on the impact of specific programming for young women only looked at single interventions. Therefore, the concept of DREAMS was that a combination of effective biomedical and structural interventions (i.e., the “layering” of services) specifically focused on the most vulnerable individual AGYW and their communities would result in collective, community-level improvements in the lives of all AGYW. PEPFAR intentionally implemented DREAMS in specific geographic areas within each country that had the highest need based on several factors, including total HIV burden, HIV prevalence among AGYW, girls’ school attendance, and rates of teenage pregnancy. In late 2015, the implementation of DREAMS began in 89 subnational geographic areas in 10 sub-Saharan African countries: Eswatini, Kenya, Lesotho, Malawi, Mozambique, South Africa, Tanzania, Uganda, Zambia, and Zimbabwe. It then expanded to five additional countries in 2017. Critically, in each country, PEPFAR engages AGYW themselves in meaningful ways at every step of the DREAMS pathway to gain and deploy their unique insights and leadership.
DREAMS has reached increasingly large numbers of AGYW across multiple, diverse settings in the 15 countries: 1.5 million AGYW in 2019 and 1.68 million in 2020. New HIV diagnoses among AGYW have declined in all geographic areas that are implementing DREAMS. Ninety-six percent of the locations have seen a decrease of greater than 25%, and nearly two-thirds (62%) experienced a drop of greater than 40%, data released on World AIDS Day 2020 show.
DREAMS has also driven a greater global focus on the unique risks and opportunities experienced by AGYW. It has pushed partner governments to renew their commitments to promote gender equality and reduce sexual violence and its impact on adolescent health and development. It has enabled multilateral organizations and nongovernmental organizations to advocate more successfully for greater attention on and investment in AGYW.
Addressing the Specific Gaps in Prevention and Treatment Services for Vulnerable Communities: The Elton John AIDS Foundation Partnership – Accelerating PEPFAR’s Response to the LGBTQ Community
A focus on the most marginalized and highly affected populations has been at the center of PEPFAR’s programming since its implementation. However, a gap in access to both prevention and treatment services has persisted in key populations around the globe. SGAC and PEPFAR implementers have learned that many of the barriers are structural, related to stigma, discrimination, the criminalization of behavior, and the violation of human rights.
Beginning in 2016, PEPFAR joined with the Elton John AIDS Foundation (EJAF) to launch the LGBT Fund, which invests in reaching key populations, including lesbian, gay, bisexual, and transgender (LGBT) people, with lifesaving HIV prevention and treatment services. The $10 million fund makes grants to peer-led organizations to address the stigma, discrimination, violence, and other violations of human rights faced by LGBT people. It has since reached nearly 60,000 LGBT people in several sub-Saharan African countries and the Caribbean through targeted, community-level projects.
This laser-focused PPP complemented an annual PEPFAR investment of $300 million for direct services to key populations under Country Operational Plans. In addition, PEPFAR’s Key Populations Investment Fund supported local organizations’ expansion of nondiscriminatory access to quality, lifesaving HIV services – and to restore health and dignity while working to control the HIV/AIDS epidemic.
At the announcement creating the LGBT Fund, Sir Elton John said: “Since I founded the Elton John AIDS Foundation a quarter of a century ago, an article of faith for us is that no one gets left behind. Our LGBT Fund in partnership with PEPFAR is part of that spirit. The LGBT community has suffered discrimination and isolation in many parts of sub-Saharan Africa, which have added to HIV vulnerability and left too many people behind in accessing treatment. I am proud of what we have achieved with this Fund and hope its work can continue.”
Addressing the Gap in Access to Treatment Services for Men: MENSTAR
Data from UNAIDS and PEPFAR programs around the world showed that PEPFAR was not adequately reaching at-risk men, particularly those between the ages of 24 and 35, with HIV treatment services. This both endangered the men’s own health and fueled the spread of HIV among AGYW. Community surveys among people ages 15 and up living with HIV also demonstrated that knowledge of HIV status, treatment coverage, and viral suppression is considerably lower for men than women. Addressing this gap and reaching men with HIV services became a high priority for PEPFAR, because epidemic control is not possible otherwise.
The MenStar Coalition, launched in 2018 at the International AIDS Society Conference in Amsterdam, is a global PPP that unites PEPFAR; the Elton John AIDS Foundation; Unitaid; the Global Fund to Fight AIDS, Tuberculosis and Malaria; the Children’s Investment Fund Foundation; Johnson & Johnson; and Gilead Sciences. The partnership specifically focuses on developing and creating demand for male friendly services by using the success and insights gained from DREAMS. Its goal is to reach men, independent of age, with lifesaving HIV services and ensure viral suppression.
MenStar’s private sector partners specifically work in communities to create demand for HIV services among young men. At the same time, PEPFAR and other partners support the expansion of male friendly services by deploying the best practices from implementing partners that were able to reach and retain men in HIV care. The partnership brings the HIV service-delivery capacities of the public sector together with the consumer-oriented marketing acumen of the private sector to optimize efforts to reach men with HIV testing and treatment services. It is an innovative way of doing business that reaches men where they are, with the services they need, when they need them. It uses a new client-centric approach of leveraging human centered design (HCD) to listen to men, identify their insights and underlying barriers, understand their emotional and health needs, and adapt HIV treatment services to meet their needs. The focus groups and data from MenStar’s private sector partners showed that, like adolescent women, men have different needs at specific points of the HIV cascade (for example, when they are undiagnosed, newly on treatment, or disengaged from care). Powered by the input of men themselves, MenStar has developed and refined innovative demand-creation and supply-side strategies to engage men and differentiate treatment services.
MenStar is constantly revising men’s relationship with health care by developing insight-driven, innovative programs to improve each stage of the HIV cascade for them. In Lesotho, MenStar has created male friendly clinics with male nurses and clinical officers that are open before and after work hours. In other countries, MenStar has worked to change laws and regulations to make HIV medication more accessible, such as the easy renewal of prescriptions and the creation of local pickup points beyond clinics. Ministries of health have allowed nurses and doctors to give clients a six-month supply of ART to decrease the time men had to take off from work and retain their privacy. In Mozambique, to address low HIV diagnosis and treatment access in men, MenStar has rebranded treatment as a solution to maintaining a normal life rather than a barrier to it.
The goal of MenStar is to reach an additional 1 million men with HIV treatment services and achieve 90% viral suppression among men to effectively interrupt HIV transmission. Since the start of the partnership, MENSTAR has added almost 2.2 million new men 15 and older onto treatment in the 21 highest-burden countries. The viral suppression among males 15 and up increased to 90% in 2019 from 88% in 2018, achieving MenStar’s stated goal, and then continued climbing to 93% in 2020 and 94% in 2021, surpassing the goal.
The data from community-level surveys taken before and after MenStar reflect these programmatic improvements. Less than 60% of men with HIV in the community were virally suppressed in a 2016-2017 survey. After MenStar, when the survey was repeated in 2020, the viral suppression was greater than 70%.
A community survey in Uganda, taken after the Ministry of Health proactively advanced male and youth friendly services, produced similar data. In less than three years, the community-level viral suppression in men increased to 69.2% from 53.6%.
Conclusion
While PEPFAR has developed and executed hundreds of PPPs over the past two decades, less-successful partnerships also have provided valuable learning experiences and identified several common factors that contribute to less-than-optimal results:
- Insufficient trust and/or communication between partners;
- Change of direction or leadership in partner countries’ governments and/or local stakeholders;
- Inability of necessary infrastructure or environmental dynamics to continue supporting the effort;
- Discontinuation of funding;
- Failure to meet the standards of the PPP as originally set forth; and
- Inability to ensure scale or quality.
The first factor identified – building and maintaining trust between partners – is perhaps the most critical and actionable. It is important to use data to drive a shared understanding of the issue at the outset of partnerships so that expectations are clearly understood. Real-time, transparent conversations are imperative from the initial negotiation of a PPP, and even more so if a project deviates from its strategy or is no longer meeting the goals of the partners. A shared understanding of the mission, critical milestones, outcomes, and desired impact is the common thread through successful PPPs.
Recommendations
The United States should learn from PEPFAR’s experience with PPPs to improve the U.S. Government’s assistance overseas:
PEPFAR
- PEPFAR and all U.S. Government global health programs need to engage actively with foundations, corporations, civil society, and other funders to ensure that host-country governments are using all possible partners in developing a national response to HIV.
- PEPFAR needs to further define specific gaps in access to diagnosis and treatment services for children. PEPFAR should consider conducting a well-powered community survey in urban and rural communities in a country with high adult treatment coverage and high adult viral suppression to understand where the missing children are, their ages and location, and recommit to programming to address the barriers that are keeping babies and children from the services they need to survive.
- PEPFAR should support, train, and empower the African private sector to create a comprehensive logistics, delivery, and supply chain as a long-term solution to meet the evolving needs of the continent.
- PEPFAR and all U.S. Government departments and agencies that implement foreign assistance for health and development should continue to actively engage private sector partners with unique and needed core competencies that complement their technical areas, including marketing, distribution networks, and information technology.
- All U.S. foreign assistance programs should, as much as possible, work with African businesses and private sector entities to further address persistent gaps and foster sustainability.
































